- Some symptoms are noticeable immediately, but other symptoms may
be milder yet still serious. - Optometrists should conduct a thorough eye examination of patients
who experience a TBI, including VA testing, ocular motility assessment,
and contrast sensitivity testing.
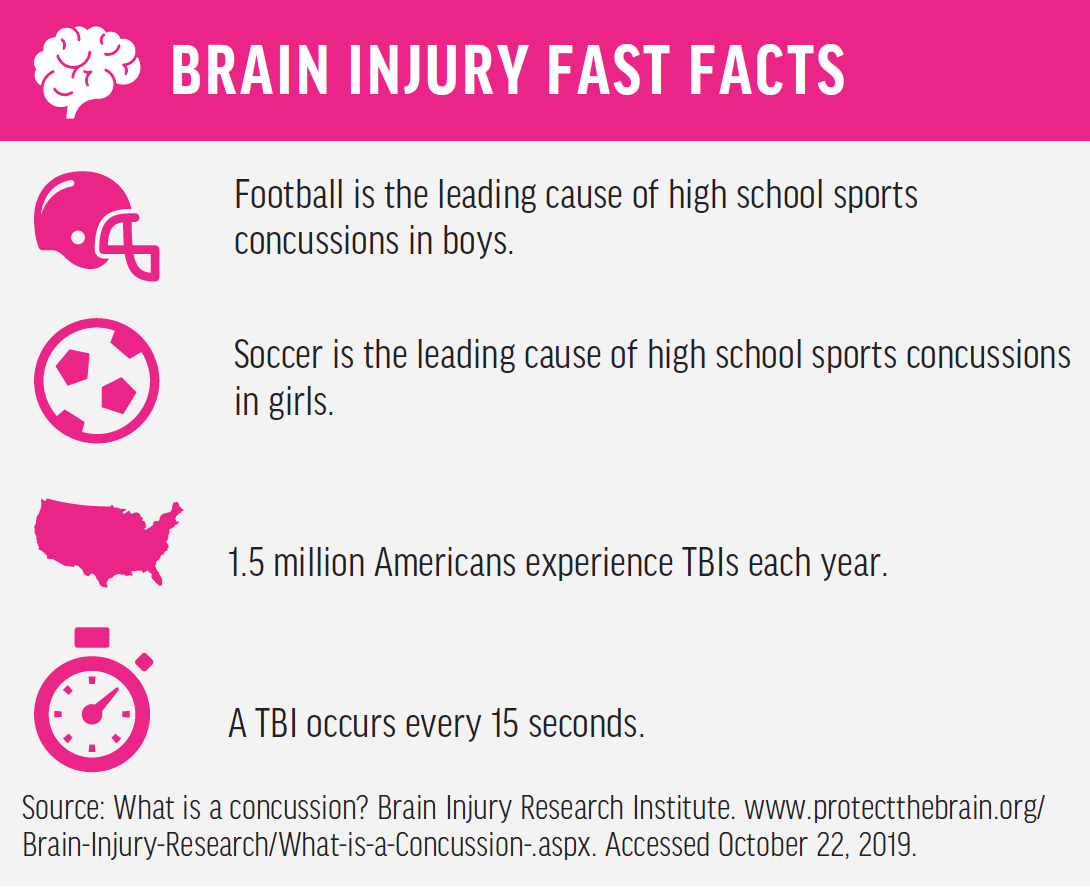
We focus on the serious and potentially fatal effects of traumatic brain injuries (TBIs). Although many people think of these types of injuries mostly in relation to football, a TBI—whether mild or severe—can occur due to multiple causes, including road accidents, trauma to head/back, etc.
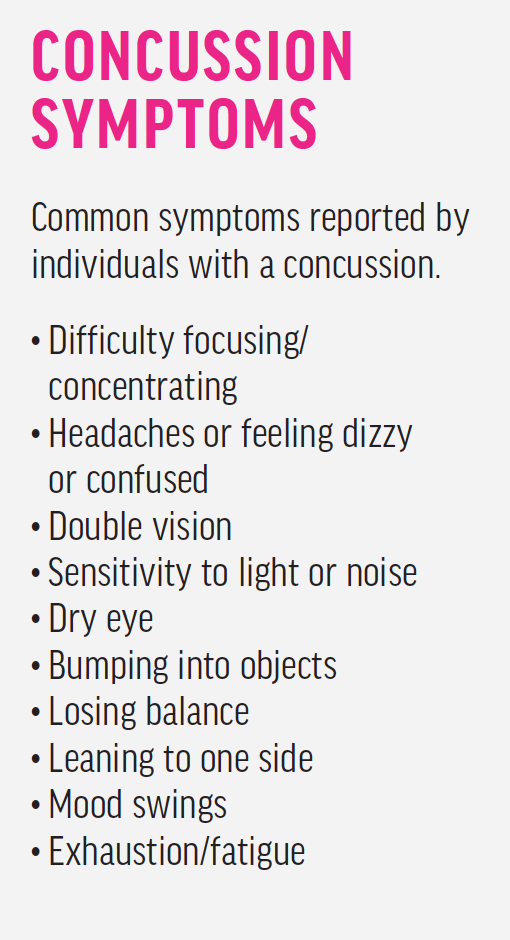
Older adolescents (ages 15–19) and older adults (ages 65 and older) are the individuals most likely to sustain a TBI. It is estimated that 3.8 million concussions occur in the United States each year, and as many as 50% of these may go unreported.1 TBIs are contributing factors to a third (30%) of injury-related deaths in the United States.2 A concussion, a mild TBI, is the most common type of TBI. Some symptoms, such as fatigue and mood swings, may not directly appear to be correlated with a head injury, whereas other symptoms are much more severe and noticeable (see Concussion Symptoms).
ASSESSMENT GUIDELINES
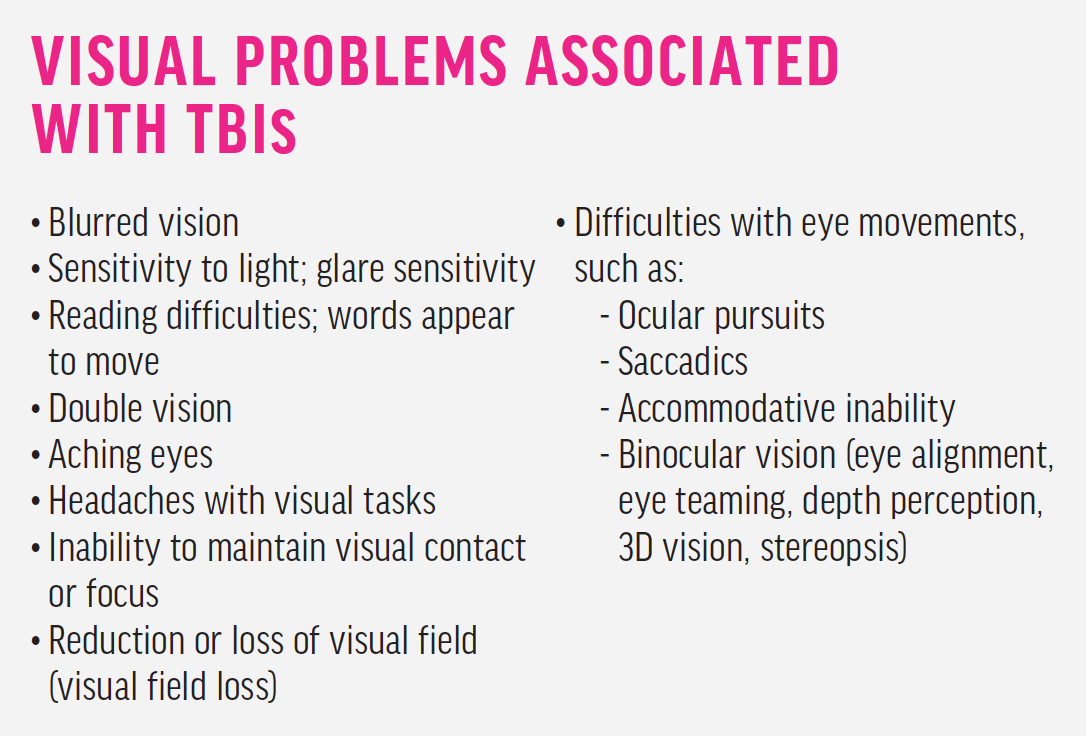
After someone experiences a TBI, it is crucial that he or she has a comprehensive eye examination along with follow-up visits. The examination should include VA testing with refraction, evaluation of pupil reactivity and color, IOP measurement, visual field testing, and dilated fundus exam. Ocular motility assessment should be conducted, including pursuits, saccades, vestibulo-ocular reflex, and convergence and divergence. Individuals with TBI may report a decrease in VA and experience foggy or blurry vision (see Visual Problems Associated With TBIs).
Neuroimaging such as a CT scan or MRI is also typically ordered; however, these scans do not always provide useful information regarding cerebral concussions. Neuroimaging should be used whenever a patient loses consciousness, experiences severe amnesia, or has increasing symptoms of headaches or nausea. If damage appears on one of these scans, the injury is more serious than a concussion.
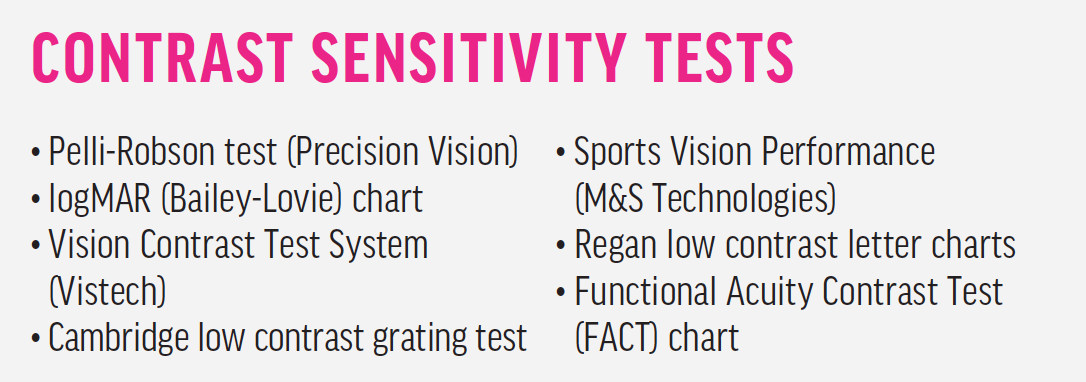
Contrast sensitivity testing is often a better predictor of functional vision than VA (see Contrast Sensitivity Tests). In contrast sensitivity testing, unlike in standard 100% contrast black-on-white VA testing, stimuli are presented against backgrounds with varying levels of contrast, giving better insight into the patient’s ability to perceive objects in the real world.
Patients with head injuries are often prescribed pain medications, and these medications can have effects on their refractive error and accommodative effort, heighten light sensitivity, and even produce color-vision defects. Patients should avoid taking medications containing aspirin, which can increase intracranial bleeding.
TREATMENT TACTICS
Treatment for concussion can take many forms. It may be as simple as changing the patient’s lens prescription. Any astigmatism should be addressed in the new prescription, as well as any hyperopia of +0.50 D or greater and myopia of -0.25 D or greater. Prescribing a second pair of reading glasses instead of bifocals can also help with accommodative issues. To help patients reduce glare issues and light sensitivity and to alleviate fatigue and daytime sleepiness, a 40% blue tint and an antireflective coating can be added to their spectacle prescription.
Another option is vision therapy, which can boost the eyes’ ability to communicate, focus, and converge and diverge. This is usually the most appropriate form of care when simple adjustments in prescription or tints are not enough.
The period of recovery after TBI can be as long as 1 to 2 years, but recovery may remain incomplete.3 Symptoms persisting beyond 1 year have been reported in 10% to 15% of those with mild TBI.4
We can recommend special supplements/medications/guidance to accelerate the healing process and sometimes 90% recovery in a much shorter time.
Although most patients with mild TBI recover to a significant degree, approximately 20% will be unable to return to work, and even more can remain symptomatic. Sensory and neurologic tracking devices can be used to improve a patient’s awareness and decision-making abilities, and these can also help determine whether an athlete can return to participating in his or her sport.
IT TAKES A TEAM
Follow-up is crucial at 1, 3, and 6 months after the injury. Treating a concussion is truly a team effort because, though some symptoms may resolve as quickly as a week, others may last years. The care team may include a neurologist, ophthalmologist, optometrist, vision therapist, occupational therapist, physical therapist, psychologist, primary care physician, speech language pathologist, and even a social worker. When everyone is included, the patient ultimately benefits.